Contents
- 1. What are spinal osteophytes?
- 2. Common Locations of Spinal Osteophytes
- 3. Who Is Susceptible to Spinal Osteophytes?
- 4. Causes of Spinal Osteophytes
- 5. Signs and Symptoms of Spinal Osteophytes
- 6. Are Spinal Osteophytes Dangerous? When Should You See a Doctor?
- 7. Can Spinal Osteophytes Be Treated?
- 8. Non-Surgical Treatment for Spinal Osteophytes
- 9. Preventing Spinal Osteophytes
Spinal osteophytes are a degenerative condition of the spine that can significantly affect a patient’s quality of life. If not detected and treated in a timely manner, spinal osteophytes may lead to severe nerve compression. In advanced cases, this condition can even result in paralysis.
1. What are spinal osteophytes?
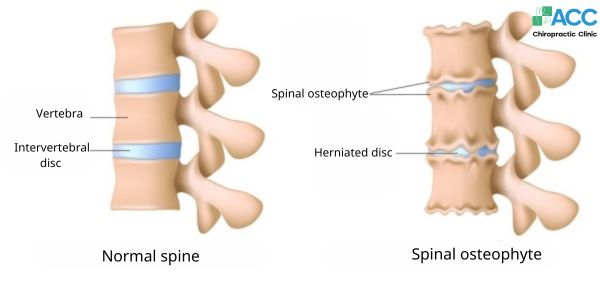
Spinal osteophytes, commonly known as bone spurs, develop as a result of spinal degeneration. These bony outgrowths typically form at areas where the vertebrae connect or experience excessive stress, including:
- The edges of vertebral bodies
- Intervertebral discs
- Spinal ligaments

Comparison images between a normal spine and a spine affected by osteophytes.
Patients with spinal osteophytes often suffer from persistent or severe pain in various parts of the body, such as the neck, shoulders, lower back, or radiating pain into the arms and legs.

2. Common Locations of Spinal Osteophytes
Spinal osteophytes can develop anywhere along the spine; however, they most commonly occur in the lumbar and cervical regions.
2.1. Lumbar Osteophytes
Lumbar osteophytes develop as a result of subchondral bone sclerosis and degeneration of the articular cartilage in the lower spine. Pain is typically localized in the central lower back and may radiate to the groin or down the legs.
2.2. Cervical Osteophytes
Cervical osteophytes are a degenerative condition affecting the cervical vertebrae. These bony growths may compress nerve roots, the cervical spinal cord, or the vertebral artery. As a result, patients may experience conditions such as:
- Cervical-shoulder syndrome
- Cervical-shoulder-arm syndrome
- Vertebral artery syndrome
- Cervical spinal cord compression syndrome
3. Who Is Susceptible to Spinal Osteophytes?
Spinal osteophytes (bone spurs) are more likely to occur in the following groups:
- Elderly individuals with age-related spinal degeneration and calcium deposits
- People who perform heavy manual labor or frequently carry heavy loads
- Individuals with poor posture while standing, walking, sitting, or sleeping
- People with a history of spinal injuries, trauma, or accidents
- Individuals who frequently consume alcohol, tobacco, or stimulants
- Patients with chronic spinal arthritis
- Overweight or obese individuals
4. Causes of Spinal Osteophytes
Identifying the underlying causes is essential for effective treatment and preventing recurrence.
In most cases, spinal osteophytes form as a result of spinal degeneration and related health conditions, including the following factors:
4.1. Calcium Accumulation
Degenerative changes cause gradual wear of bones and joints, leading to abnormal calcium deposition (such as calcium pyrophosphate). This excessive accumulation contributes to the formation of bone spurs.
4.2. Spinal Injury
The body has a natural self-healing mechanism following injury, including injuries to the spine. During this process, the body may increase calcium deposition at the damaged site to repair lost tissue. Over time, this compensatory response can unintentionally lead to the development of spinal osteophytes.

4.3. Chronic Arthritis
Similar to spinal injuries, long-term arthritis leads to progressive cartilage erosion. To compensate for this damage, the body increases calcium deposition around the affected joints. Over time, this excessive calcium buildup results in the formation of bone spurs, leading to spinal osteophytes.
Overall, the primary causes of spinal osteophytes originate from conditions that damage spinal structures. In addition, several other health-related factors may contribute to the development of this condition, including:
- Autoimmune and metabolic disorders such as lupus and gout
Obesity - Genetic predisposition (poor disc health from birth)
- Poor posture during daily activities such as walking, sitting, studying, or sleeping
4.4. Spinal Degeneration
Spinal degeneration is one of the leading causes of bone spur formation. Degenerative changes make spinal cartilage more vulnerable to cracking and breakdown. When this occurs, the body activates its natural repair mechanism by depositing calcium into the damaged areas. However, uneven or excessive calcium deposition may occur, creating areas of calcium imbalance. Over time, this process leads to the gradual formation of spinal osteophytes.
5. Signs and Symptoms of Spinal Osteophytes
The most common symptoms of spinal osteophytes include pain and discomfort in one or more areas of the body—such as the neck or back—especially during movement.
- Signs of Lumbar Spinal Osteophytes
- Lower back pain that may radiate to the legs or groin
- Pain persisting for more than six weeks
- Increased pain when sitting for prolonged periods, turning over, or bending
- Difficulty controlling bladder or bowel function
- Loss of balance; patients may tend to lean forward or backward
- Signs of Cervical Spinal Osteophytes
- Dull, aching pain in the neck, which may worsen with sudden movements or weather changes
- Numbness, soreness, and stiffness in the neck and shoulders
- Neck stiffness with limited range of motion, difficulty turning the head side to side
- Headaches with throbbing pain radiating to the top of the head
- Dizziness, nausea, fatigue, and general discomfort
To accurately diagnose Spinal Osteophytes and assess the severity of the condition, imaging studies such as X-rays are typically required under a physician’s evaluation.
6. Are Spinal Osteophytes Dangerous? When Should You See a Doctor?
If Spinal Osteophytes are not treated early, they can negatively affect the spinal cord and surrounding nerves, leading to serious complications, including:
Spinal stenosis: Newly formed bone spurs may encroach on the spinal canal, narrowing the space available for nerves. This can cause localized pain, along with numbness and weakness in the arms or legs.
Paralysis and loss of working ability: Prolonged nerve compression can gradually impair nerve function, potentially leading to partial or complete paralysis.
Vestibular disorders: These complications commonly occur in patients with cervical spine degeneration. Reduced blood and oxygen flow to the brain may result in dizziness, nausea, balance problems, and other vestibular symptoms.
Other complications: Blood pressure fluctuations, scoliosis, sleep disturbances, and chronic fatigue.
For these reasons, doctors strongly recommend seeking medical evaluation if you frequently experience pain, swelling, or stiffness in the neck, back, hips, or legs, especially when accompanied by difficulty moving.

7. Can Spinal Osteophytes Be Treated?
To relieve pain and restore function, patients should consult a physician to determine the most appropriate treatment approach. Current treatment options include:
7.1. Gentle Exercise
Light activities such as cycling, yoga, swimming, and walking may help reduce pain and stiffness. However, this approach mainly provides temporary relief and should be combined with other therapies for better long-term outcomes.
7.2. Physiotherapy
In many countries such as the United States, Germany, and the United Kingdom, patients increasingly prefer non-invasive treatments like physiotherapy. This method is considered safe and effective, combining modalities such as shortwave therapy, infrared therapy, and structured rehabilitation exercises to improve spinal function.
7.3. Western Medications
Doctors may prescribe medications to help relieve pain, including:
- Acetaminophen (paracetamol)
- Ibuprofen
- Naproxen

However, these medications only offer temporary symptom relief. Prolonged or frequent use may cause side effects such as gastrointestinal ulcers, high blood pressure, osteoporosis, cataracts, or allergic reactions, especially in individuals sensitive to certain drugs.
7.4. Traditional Medicine Remedies
Some patients choose herbal or traditional remedies to alleviate symptoms of Spinal Osteophytes. While these methods may provide short-term relief, self-medication with unverified products can lead to serious complications such as liver and kidney damage, metabolic disorders, or even life-threatening conditions.
7.5. Surgery
Surgery may be considered in severe cases or when conservative treatments fail. However, it is generally not the preferred option because:
- The risk of complications during and after surgery is relatively high
- Surgery mainly relieves symptoms; bone spurs may recur or new spurs may form
- High treatment costs make surgery inaccessible for many patients
8. Non-Surgical Treatment for Spinal Osteophytes
Pain associated with Spinal Osteophytes primarily results from structural misalignment and nerve compression. Chiropractic care aims to correct spinal misalignment, reduce nerve pressure, and address the root cause of pain—making it a preferred non-surgical option for many patients.

In Vietnam, ACC Clinic, specializing in Chiropractic care, is proud to be a pioneering center in applying this treatment approach. To enhance recovery, ACC doctors combine Chiropractic treatment with modern physiotherapy and rehabilitation techniques, such as:
- Spinal decompression using DTS technology
- Shockwave therapy
- High-intensity laser therapy (Generation IV)
- In addition, patients receive personalized nutritional advice and guided exercise programs to help prevent recurrence.
9. Preventing Spinal Osteophytes
- To reduce the risk of developing Spinal Osteophytes, you should:
- Increase intake of fiber, vitamin D, and other essential nutrients
- Quit smoking and limit foods that contribute to weight gain
- Avoid prolonged sitting
- Refrain from strenuous activities (heavy weightlifting, intense gymnastics, excessive push-ups)
- Avoid lifting heavy objects improperly
At the first sign of unusual spinal symptoms, seek medical evaluation promptly to ensure early diagnosis and appropriate treatment.
>> Related post: Disc syndrome and information you should not pass